What Is The Test For Scoliosis? Understanding Your Diagnosis

The most important part of a scoliosis diagnosis is how it's responded to with treatment, and understanding your diagnosis means understanding how conditions are classified. Conditions are classified based on key variables and treatment plans are shaped around them.
Scoliosis is a prevalent spinal condition that's diagnosed through a physical examination, an Adam's forward bend test, and X-ray results. Together, a complete picture of what is happening in and around the spine can be given.
There are a number of spinal conditions that cause a loss of healthy spinal curves, but scoliosis has some unique characteristics.
Table of Contents
Understanding Scoliosis
Scoliosis is a spinal condition affecting approximately seven million people in the United States alone, and as the leading spinal condition among school-aged children, scoliosis screening is important.
Scoliosis causes the spine to bend unnaturally to the side and rotates, making it a complex 3-dimensional condition.
Scoliosis is also a progressive spinal condition, so its nature is to get worse over time, and this involves the unnatural spinal curvature getting larger, and as this occurs, the condition's effects become more severe and overt.
The more scoliosis progresses, the more difficult it can be to treat.
Diagnosing a complex condition like scoliosis isn't simple because no two cases are the same, and this is why the diagnostic process involves further classifying conditions based on key variables that vary from patient to patient.
Scoliosis ranges widely in severity from mild scoliosis to moderate scoliosis, severe and very severe scoliosis.
There are also different types of scoliosis with various causes and treatment needs, and also different curvature types, patterns, and locations within the spine.
Diagnosing scoliosis involves a comprehensive physical examination and assessment.
Diagnosing Scoliosis: Adam's Forward Bend Test
 The first step of a diagnosis involves assessment and a physical examination.
The first step of a diagnosis involves assessment and a physical examination.
Taking the patient's family history and medical history are part of the assessment, and the most commonly-used scoliosis screening exam is known as the Adam's forward bend test.
An Adam's forward bend test involves having the patient bend forward at the hips as if trying to touch the toes, and examining the back and spine in this position makes any unnatural curves and trunk asymmetries highly visible.
Scoliosis introduces a lot of uneven forces to the spine and body that can disrupt the body's overall symmetry, and trunk asymmetries such as uneven shoulders, uneven shoulder blades, uneven hips, and the development of a rib cage arch are common.
An Adam's forward bend test, when combined with the use of a scoliometer, looks for indicators of scoliosis and a patient's angle of trunk rotation (ATR).
If the Adam's test has shown indicators of the condition, this doesn't guarantee a scoliosis diagnosis but does warrant further testing, in the form of a scoliosis X-ray.
Scoliosis X-Ray
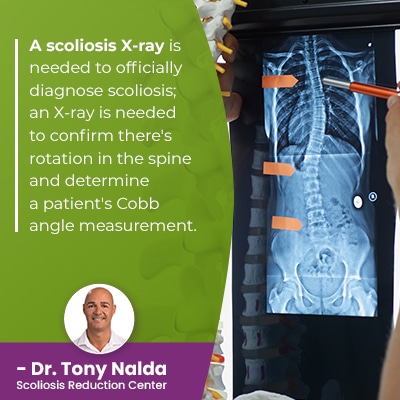
A scoliosis X-ray is needed to officially diagnose scoliosis; an X-ray is needed to confirm there's rotation in the spine and determine a patient's Cobb angle measurement.
A minimum Cobb angle of 10 degrees is needed to reach a diagnosis of scoliosis.
A patient's Cobb angle measurement is determined by drawing lines from the tops and bottoms of the curve's most-tilted vertebrae at its apex.
The more unnaturally-tilted the vertebrae are, the higher the Cobb angle, the more severe a condition, and the more complex it will be to treat.
- Mild scoliosis: Cobb angle measurement of between 10 and 25 degrees
- Moderate scoliosis: Cobb angles of between 25 and 40
- Severe scoliosis: Cobb angle of 40+ degrees
- Very-severe scoliosis: Cobb angle of 80+ degrees
And, remember, as a progressive condition, where a patient's scoliosis is at the time of diagnosis doesn't mean that's where it will stay.
So through the diagnostic process, conditions are assessed and classified based on key variables, and these variables shape the customization of treatment plans.
Classifying Scoliosis
Scoliosis is classified based on key patient/condition variables, and treatment plans are shaped around addressing each variable.
Patient age, condition severity, type, and curvature location are important for different reasons.
Patient Age
Patient age is important not just because it indicates overall health and spinal flexibility but also because scoliosis progression is triggered by growth, so children are the most at risk for continued and rapid progression.
Adolescent idiopathic scoliosis is the most prevalent type of scoliosis overall, and adolescents are the most at risk for rapid-phase progression due to the rapid and unpredictable growth spurts of puberty.
Patient age is also important when it comes to factoring in whether or not pain management has to be a focus of treatment.
Scoliosis doesn't become a compressive condition until skeletal maturity has been reached; it's compression (uneven pressure) that causes the majority of condition-related pain.
Compression doesn't just affect the spine, but also its surrounding muscles and nerves.
While pain is the main symptom of adult scoliosis, postural changes are the most common signs of scoliosis in children.
So pain management has to be factored into most adult scoliosis treatment plans, but isn't a common focus in childhood scoliosis treatment.
Condition Severity
Condition severity, as mentioned, is determined by a patient's Cobb angle measurement.
Condition severity is a key piece of information because it indicates how much progression has occurred, and the more severe a condition is, the more likely continued progression is.
Mild curves are simpler to treat than moderate and severe curves, so the goal is if a condition is diagnosed while mild, to keep it that way; only proactive treatment can work towards counteracting the condition's progressive nature.
There are never treatment guarantees, but in most cases, the sooner treatment is started, the better.
Condition Type
Condition type is determined by causation, and in the majority of scoliosis cases, we don't know why they initially develop, and this type is known as idiopathic scoliosis.
Idiopathic scoliosis has no known cause but accounts for approximately 80 percent of known cases, and the remaining 20 percent consist of known causes: neuromuscular, degenerative, and congenital.
Condition type is an important factor because different condition types have unique characteristics and treatment needs.
In most typical cases of idiopathic scoliosis, curves bend to the right, away from the heart, but in atypical cases with known causes, curves can bend to the left, towards the heart; this is why an X-ray is needed to diagnose scoliosis and see what's really happening to the spine.
Neuromuscular scoliosis is caused by the presence of a larger neuromuscular condition like spina bifida, muscular dystrophy, and cerebral palsy.
Degenerative scoliosis affects older adults and is caused by natural age-related spinal degeneration.
Congenital scoliosis is caused by a malformed spine that develops in utero.
Curvature Location
 There are three main spinal sections: the cervical spine (neck), thoracic spine (middle/upper back), and the lumbar spine (lower back).
There are three main spinal sections: the cervical spine (neck), thoracic spine (middle/upper back), and the lumbar spine (lower back).
Scoliosis can develop in any of the spine's main sections, or in more than one, as a combined scoliosis.
Curvature location can also be determined on X-ray, and it's important because it indicates the types of symptoms a patient is likely to experience, along with indicating where treatment efforts need to be concentrated.
In most cases, the area of the body located closest to an affected spinal section is the area that's going to feel the majority of the condition's direct effects.
So curvature location is another key factor that's determined during the diagnostic process.
Conclusion
While some childhood scoliosis screening still occurs in schools, it occurs less than in the past, shifting the onus of early detection and intervention onto the shoulders or parents, caregivers, and patients themselves.
There are never treatment guarantees, but because scoliosis is progressive, there are always advantages to starting treatment early, and there is a direct link between early detection and treatment success.
While there is no single test for diagnosing scoliosis, through a combined physical examination and X-ray results, conditions can be diagnosed based on the presence of an unnatural sideways-bending spinal curve with rotation and a minimum Cobb angle of 10 degrees.
Once a diagnosis is reached, it's important for patients to understand that there is more than one way to treat scoliosis, and knowing the difference means understanding how each affects long-term spinal health.
While traditional treatment would follow a diagnosis of mild scoliosis with a recommendation to watch and wait for continued progression, modern conservative treatment has a proactive approach.
As progressive conditions are virtually guaranteed to progress at some point, watching and waiting is wasting valuable treatment time, and remember, the more a condition progresses, the more complex it is to treat.
Abnormal spinal curvatures are simpler to correct early in their progressive line, and while surgical treatment is commonly recommended for severe and very severe cases, proactive treatment can work towards preventing progression.
Here at the Scoliosis Reduction Center®, patients benefit from proactive non-surgical treatment options that work together to prevent progression, reduce curve size, and improve the spine's balance and alignment.
Dr. Tony Nalda
DOCTOR OF CHIROPRACTIC
After receiving an undergraduate degree in psychology and his Doctorate of Chiropractic from Life University, Dr. Nalda settled in Celebration, Florida and proceeded to build one of Central Florida’s most successful chiropractic clinics.
His experience with patients suffering from scoliosis, and the confusion and frustration they faced, led him to seek a specialty in scoliosis care. In 2006 he completed his Intensive Care Certification from CLEAR Institute, a leading scoliosis educational and certification center.
About Dr. Tony Nalda
 Ready to explore scoliosis treatment? Contact Us Now
Ready to explore scoliosis treatment? Contact Us Now





